Find out about financial assistance for lemtrada
patients
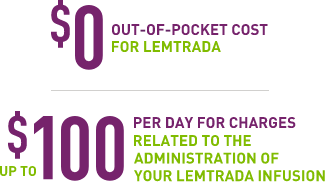
To help make your relapsing MS treatment costs and co-pays more affordable, we created the
LEMTRADA Co-Pay Program. Through the program, financial assistance is available to help eligible*,
commercially insured patients receive LEMTRADA with:

How to Enroll
- First, find out if you’re eligible for financial assistance. Call 1-855-676-6326. Support is
available 24/7.† - If you have commercial insurance, you may be eligible through the LEMTRADA Co-Pay
Program. - You will be contacted by an MS One to One® Case Manager from our service center
who will explain the benefits of the program. -
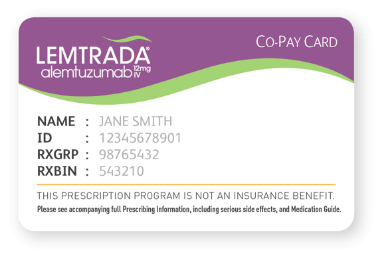
You will receive a LEMTRADA Co-Pay Card by mail, with instructions on how to submit
for benefits. Whenever you submit a bill or Explanation of Benefits (EOB), you will need
to reference the member ID number on your card. - If your healthcare facility is submitting for you, be sure to give them a copy of your
LEMTRADA Co-Pay Card.
How to submit your claim
Your health plan automatically sends you the EOB after you receive your treatment. Once you receive the EOB, you can submit for your co-pay benefit in one of two ways:
-
Your doctor’s office or healthcare facility submits a detailed copy of the EOB or your bill to the LEMTRADA Co-Pay Program. Confirm if they will be submitting and provide them with a copy of your LEMTRADA Co-Pay Card.
The LEMTRADA Co-Pay Program then verifies your information, and once it is confirmed, we will send a check to your healthcare facility or doctor’s office within 7 to 10 days. The check will cover the cost of the out-of-pocket, drug-related charges only. Our program also covers up to $100 a day for infusion-related charges. If the healthcare facility hasn’t received a check 14 business days after a claim has been submitted, please tell them to call MS One to One at 1-855-676-6326.
-
You may also submit a detailed copy of the EOB or your bill along with the information provided on your LEMTRADA Co-Pay Card. They may be faxed to 1-855-557-2478 or mailed to PO Box 220790, Charlotte, NC 28222-0790.
The LEMTRADA Co-Pay Program then verifies your information, and once it is confirmed, a check will be sent to you within 7 to 10 business days. The check will cover the cost of the out-of-pocket, drug-related charges only. Our program also covers up to $100 a day for infusion-related charges. If you haven’t received a check 14 business days after a claim has been submitted, please call MS One to One at 1-855-676-6326.
- Receive your infusion.
- Have the specialty pharmacy fax a copy of your detailed EOB to 1-855-557-2478.
- The LEMTRADA Co-Pay Program verifies your information. After all required information is confirmed, only the drug-related charges will be paid.
- Your healthcare facility can submit an EOB to the LEMTRADA Co-Pay Program to receive the benefit of up to $100 per day for infusion-related, out-of-pocket charges.
- You may also submit a detailed copy of the EOB or a copy of the healthcare facility’s bill along with the information provided on your LEMTRADA Co-Pay Card.
- Note: This program helps pay for drug costs described as “out-of-pocket,” “co-pay,” “co-insurance,” or “uncovered expense” for LEMTRADA only, and up to $100 for other costs related to the infusion.
*Patients who have coverage or prescriptions paid for in part or in full under Medicare, Medicaid, or other state or federally funded healthcare programs are not eligible. The LEMTRADA Co-Pay Program is subject to termination or modification at any time. If you are not eligible for the LEMTRADA Co-Pay Program and need help with out-of-pocket expenses, MS One to One can help review your coverage options. Depending on your specific situation, your MS One to One Case Manager can direct you to other patient assistance programs that may offer you financial support. Treatment-related, infusion out-of-pocket costs are not reimbursable in MA, MI, or RI.
†As a member of MS One to One, you’ll have access to an on-duty Case Manager 24/7. Regular MS One to One call center hours are Monday–Friday, 8:30 am–8:00 pm ET.
Sanofi reserves the right at any time and without notice to modify or change eligibility criteria or discontinue this program.
LAB
Testing at any LabCorp® or Quest Diagnostics™ patient service centers.
HEALTHCARE PROVIDER’S OFFICE
Samples can be taken at your healthcare provider’s office.
Sanofi reserves the right at any time and without notice to modify or change eligibility criteria or discontinue this program.
Trademarks not owned by Genzyme Corporation or Sanofi are the property of their respective owners.


